PHAGES AGAINST MULTIDRUG-RESISTANT BACTERIA
Multi-resistant germs pose a consistent threat to our healthcare system. For example, a recent study published in The Lancet shows that approximately 4.95 million of the worldwide deaths in 2019 may be linked to antibiotic-resistant germs (1). It is estimated that this number could increase to approximately 10 million by the year 2050 (2).
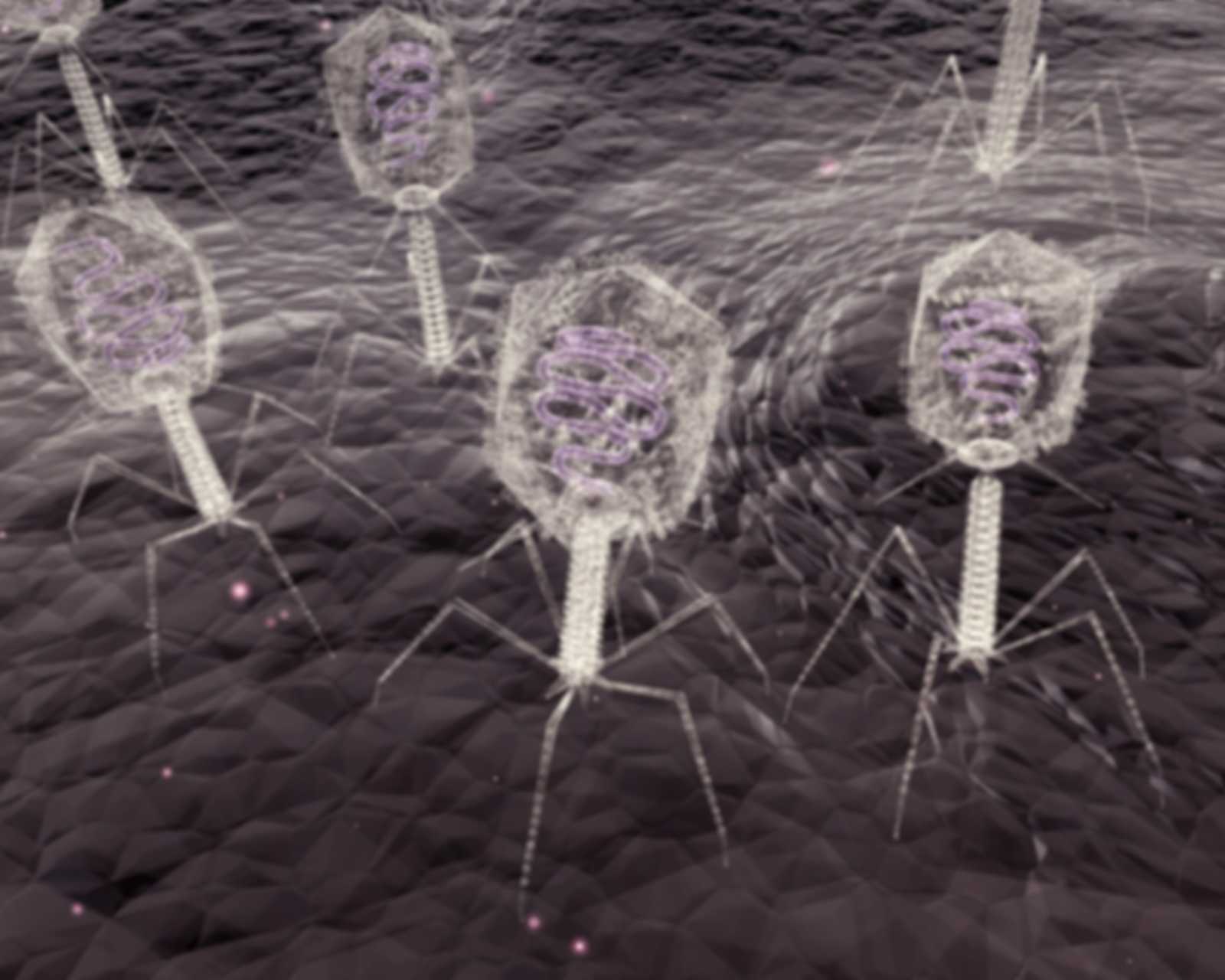
The current evolutionary resistance of these germs to antibiotics means that developing alternative forms of therapy is becoming more important than ever. One alternative could be bacteriophages. Unlike antibiotics, bacteriophages are not active ingredients but active viruses that only infect bacteria—which therefore makes their approval as a drug in Germany and the EU more difficult. Bacteriophages are so specifically adapted to their host bacteria that they do not even attack closely related bacterial strains. Because of how they work, bacteriophages are considered self-limiting and have very few side effects (3).
Phage therapy has existed for over 100 years, but it has had difficulty becoming an established, useful alternative to antibiotics because of its complexity. In the wake of increasing antibiotic resistance, research into the bacteriophage’s mode of action, diagnostics, and ultimately, their translation into the clinic has become enormously important for bringing them to market in a timely manner as an alternative, drug-based therapy. By this time, there are numerous groups in Germany and Europe with different research focuses that should be considered more closely and examined for innovative approaches.
Content and goals according to validation contract
Currently, although these research groups are working based on jointly formulated goals, they are mostly doing so independently of and uncoordinated with each other. On their own, each group is gaining important knowledge and contributing to the implementation of bacteriophage applications against multidrug-resistant bacteria, and their internal networking continues to make headway. However, overall coordination between the groups could enhance and speed up results. That is why SPRIND has commissioned Prof. Dr. Christian Willy and Dr. Felix Bröcker to develop a step-by-step concept for establishing a center for bacteriophage research, application, and production in Germany by 2030.
Prof. Dr. Christian Willy from the Federal Armed Forces Hospital Berlin has worked for years as Clinic Director of the Clinic for Trauma Surgery and Orthopedics, where he has been using bacteriophages to treat patients in individual healing trials. He is head of consortium of the PhagoFlow project and has been involved and recognized in the bacteriophage community for years. He is supported by Dr. Felix Bröcker, who, through his many years of work as a virologist and microbiologist in academic and industrial research, is familiar with both the scientific and economic aspects of drug development.
A detailed summary of the results of this assignment are now available in English and for download here.
(1) Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022 Feb 12;399(10325):629-655. doi: 10.1016/S0140-6736(21)02724-0. Epub 2022 Jan 19. Erratum in: Lancet. 2022 Oct 1;400(10358):1102. PMID: 35065702; PMCID: PMC8841637.
(2) Tackling drug-resistant infections globally: final report and recommendations / the Review on Antimicrobial Resistance chaired by Jim O'Neill. Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
(3) Liu D, Van Belleghem JD, de Vries CR, Burgener E, Chen Q, Manasherob R, Aronson JR, Amanatullah DF, Tamma PD, Suh GA. The Safety and Toxicity of Phage Therapy: A Review of Animal and Clinical Studies. Viruses. 2021 Jun 29;13(7):1268. doi: 10.3390/v13071268. PMID: 34209836; PMCID: PMC8310247.



